"Fast Pass" to stroke recovery
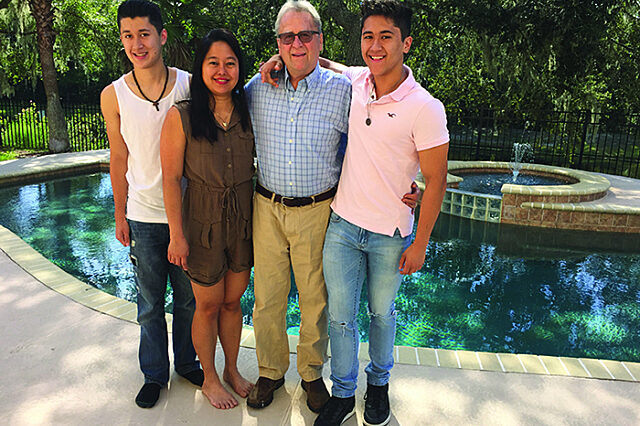
The Susdorf family pictured at their home.
Just after sunset on June 11, 2018, Joseph Susdorf stood at the entrance of Jacksonville International Airport, tapping his right hand but feeling nothing. In the short walk from the parking garage, a nagging numbness developed into a dead hand. The sensation quickly spread down his body.
Joseph collapsed to one knee and heard a police officer say, “He’s having a stroke,” before everything went black.
Meanwhile, waiting in the baggage claim area, Joseph’s wife, Charoline, was growing concerned. He had dropped her off to greet her visiting family while he parked the car. What was taking so long?
The police officer answered Joseph’s ringing cell phone and guided Charoline to the scene. She found him sprawled out, physically conscious but mentally unaware.
“His skin was pale and clammy, and his mouth drooped,” she remembered. Screaming through tears, she tried to rally a response. “I called out his name and asked if he knew me. His eyes were blank. He tried to speak, but no words came out.”
An ambulance whisked Joseph to UF Health Jacksonville. More flashing lights followed, with a police escort for Charoline and her family. “Within minutes, a doctor told me, ‘I need your permission to administer tPA,’” she said.
tP-what?
Known as a clot-buster, tissue plasminogen activator dissolves the blood clots that cause ischemic strokes. These strokes account for 85 percent of strokes each year in the United States. There is only a four-and-a-half-hour window to administer the medication following the onset of a stroke. Scared and confused, Charoline relied on the medical staff to help her decide.
“How good is it?” she asked. The doctor said, “One in three recover.”
She signed the paperwork.
Immediate treatment can be life-changing, says Scott Silliman, MD. “A clot in an artery on the left side of the brain has potential to leave someone unable to speak or to understand,” he said. “Unable to read or write as well.”
Stroke care from a stroke care innovator
Silliman is a founding physician and the current director of the UF Health Comprehensive Stroke Program. He arrived at the hospital 22 years ago — the same year tPA gained FDA approval.
The professor of neurology participated in a pre-approval clinical trial for tPA in the early 1990s and keeps an original tPA medication bottle displayed in his office. A white label containing medical jargon scripted by an electronic typewriter validates its contents as well as its age.
The souvenir contains only a few droplets, a progenitor to the fluid used to save Joseph.
Neurology specialist Nikola Jovanovic, MD, and a team of emergency room physicians and staff acted quickly, administering tPA through an IV in Joseph’s arm.
“The tPA went in and blasted part of the clot out,” Joseph said, bringing his fingers together on his forehead and quickly snapping them out. “After that? Bang. My right arm and leg popped up.”
Because a remaining portion of the clot continued to obstruct a cerebral artery, Joseph qualified for a thrombectomy.
“It’s a new strategy,” Silliman said. The clinical trials were published in the New England Journal of Medicine just two years earlier. “Adding clot retrieval to tPA in certain patients has changed the landscape of recovery. The two-step strategy results in an overall reduction in disability compared with intravenous tPA alone.”
During the procedure, Dan Siragusa, MD, chief of interventional radiology, and his team guided a catheter that contained a stent-based retrieval device through Joseph’s circulatory system and extracted the remainder of the clot from the brain artery.
“They went into an artery,” Joseph said, pointing to his inner thigh. He wrapped his left hand around his right-hand fingers, then yanked them out with force. “They sucked everything out that they blew apart.”
Other plans
Joseph does not remember any of it firsthand. Doctors said he was awake throughout the procedure, though not alert. His first memory is Charoline by his side in the Neuro Intensive Care Unit.
“I told her, we’ve got to get out of here.”
Plans had been made for the visiting in-laws.
“We need to get to Disney World.”
Michael Pizzi, MD, who specializes in neurocritical care, and his team closely monitored Joseph over the next three days.
“Blood vessels can break, and hemorrhage in the brain can occur in some patients following tPA treatment and/or clot retrieval if their blood pressure is not kept below certain parameters,” Pizzi said.
Once Joseph moved from intensive care to another unit, the neurology team found that he had an irregular heartbeat called atrial fibrillation. This condition is associated with a higher risk of clot formation within an upper heart chamber, the likely cause of Joseph’s stroke. An oral medication that thins the blood was prescribed to reduce the risk of future stroke.
“I was really impressed with his wife,” Silliman said. “Charoline was on board with continuing his care at home from the start.”
After five days at UF Health Jacksonville, Joseph made good on his promise to the visiting family members. He spent one night in his own bed, then got up early the next morning and took them to Disney World.
About the author
